There isn’t a more dangerous phrase in healthcare than “but that’s the way I’ve always done it!” There is nothing that hurts my ears more than hearing this phrase. As I’ve said before, in healthcare, the one thing you can count on is change. And oh, boy, is rapid change heading our way.
By neglecting to stay on top of all the legislative changes, you risk noncompliance with regulations, which can result in fines, deficiencies during survey, resident injuries, and now reimbursement penalties. CMS could not be more transparent: they do not want preventable readmissions. If you haven’t made changes in your processes, you’re already behind. The performance measurement period for VBP was almost 2 years ago (CY2015).
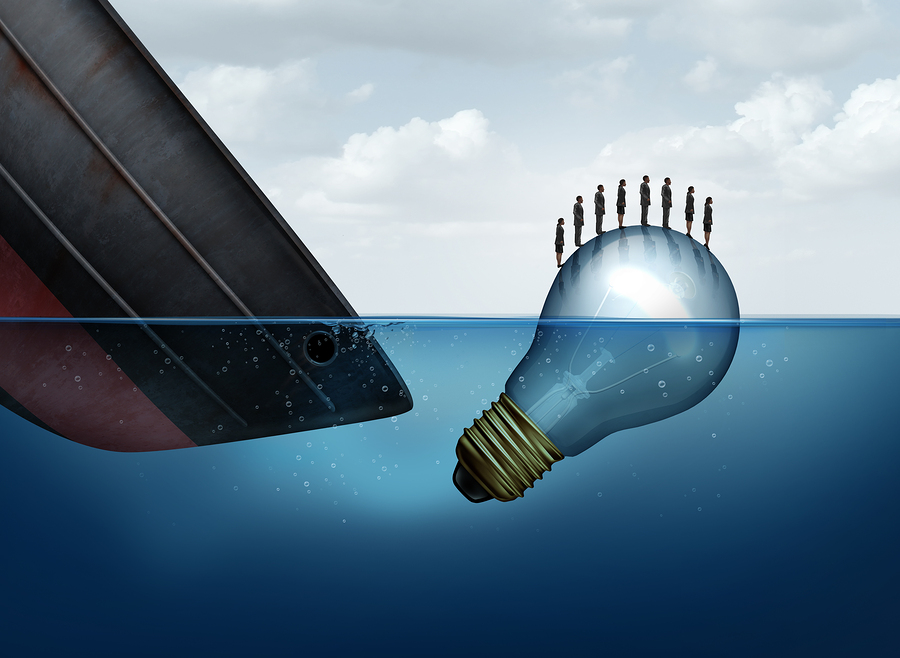
Let’s examine one process that should have evolved with the times…
Home visits.
Traditionally, home visits have occurred close to discharge from a SNF when a resident is heading home. The same risk that caused the admission sometimes was not addressed until the resident was heading out the door, going home. (Think Einstein’s definition of insanity here.)
Let’s reframe the same scenario with more coordination of care. The resident transitioned from an acute care setting to the next level of care at a SNF; home visit is scheduled within the first 48 hours of arriving at SNF; staff readily identifies areas which need to be addressed and repaired prior to patient safely transitioning back home; goal is to remove the barriers and address all safety needs. This allows for ample time to train the resident and their family on safe practices. Simple change in timing of a home visit can prevent recurrence and potential readmission.
Partnerships should be developed with all care providers across the continuum of care. Each episode of care may encounter an ER visit, a hospital stay, transition to PAC, and home care.
The goal is seamless transition of care, sharing of information, shared responsibilities, and shared results.
Create communication tools with your preferred networks. Make sure that you are measuring what is important to your payers and your partnerships.
Einstein’s definition of insanity: continuing to do the same thing and expecting a different outcome.

Comments (0)